💊 Vitamins
Nutrients
Biochemistry
October 28, 2025
Share
Vitamin D is a fat-soluble secosteroid hormone (hormone made from cholesterol) that is essential for bone health. Its active form, 1α,25-dihydroxyvitamin D (calcitriol) binds to the vitamin D receptor (VDR – a receptor inside the cell nucleus that controls gene expression). When calcitriol binds VDR, the receptor pairs with another nuclear receptor called RXR (retinoid-X receptor – activated by vitamin A).
This VDR–RXR complex attaches to DNA and switches on genes involved in calcium and phosphate absorption, bone building, and bone remodelling.
Calcitriol stimulates the activity of osteoblasts (bone-forming cells), promoting their maturation and increasing the production of structural bone proteins such as collagen, alkaline phosphatase (ALP – an enzyme needed for bone mineralisation), and osteocalcin (a protein that binds calcium into bone).
At the same time, calcitriol also influences osteoclasts (bone-resorbing cells) indirectly. When VDR is activated in osteoblasts and osteocytes, these cells produce RANKL (Receptor Activator of Nuclear Factor-κB Ligand – a signalling molecule that activates osteoclasts).
RANKL binds to RANK receptors on osteoclast precursors (immature bone-resorbing cells) and stimulates osteoclastogenesis (the formation and activation of osteoclasts).
Because vitamin D can increase both bone matrix formation (osteoblast-driven) and bone resorption (via RANKL activation of osteoclasts), its effect on the skeleton depends on mineral availability and cofactors. With adequate calcium, magnesium, and vitamin K₂, vitamin D signals bone formation; without them, it can increase bone resorption.
Vitamin D Synthesis and Metabolism
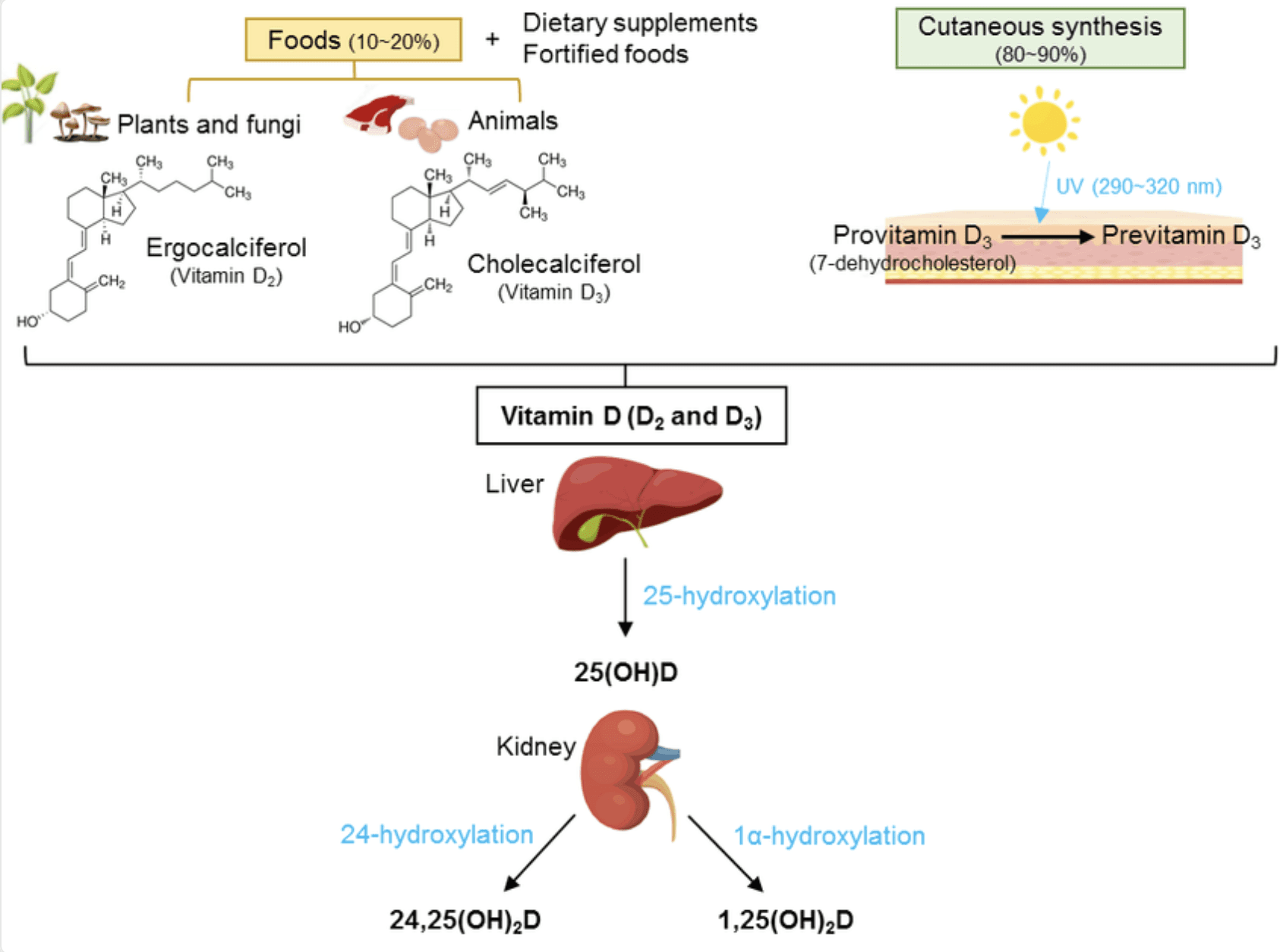
Skin synthesis
Ultraviolet-B light (290–320 nm) converts 7-dehydrocholesterol (a cholesterol derivative) in the skin into pre-vitamin D₃, which naturally rearranges into vitamin D₃ (cholecalciferol). Excess UV converts surplus into harmless inactive forms, preventing overdose from sunlight.
Transport
Vitamin D₃ travels in the bloodstream bound to DBP (vitamin D-binding protein) until it reaches the liver.
Liver conversion (25-hydroxylation)
Liver enzymes (CYP2R1, CYP27A1, CYP3A4) convert vitamin D₃ into 25-hydroxyvitamin D [25(OH)D], the main storage form measured in blood tests.
Kidney activation (1α-hydroxylation)
25(OH)D is converted into the active hormone 1,25-dihydroxyvitamin D (calcitriol) by the kidney enzyme CYP27B1.
Stimulated by PTH (parathyroid hormone – released when calcium is low)
Inhibited by FGF23 (fibroblast growth factor-23 – regulates phosphate)
Breakdown (catabolism)
When vitamin D levels are high, or calcium is abundant, the hormone FGF23 (fibroblast growth factor-23) activates CYP24A1.
CYP24A1 then converts vitamin D into 24,25(OH)₂D, which is eventually excreted.
Local activation in tissues
Many tissues, including bone and immune cells, can locally convert 25(OH)D to calcitriol for autocrine/paracrine use (local communication between nearby cells).
How Vitamin D Works Through VDR
Once inside the nucleus:
Calcitriol binds VDR (vitamin D receptor)
VDR pairs with RXR (vitamin A-dependent co-receptor)
The VDR–RXR complex binds VDREs (vitamin D response elements – gene switches)
This activates genes responsible for:
calcium/phosphate uptake from the gut,
production of bone-matrix proteins,
regulation of RANKL and OPG (osteoprotegerin – a decoy receptor that blocks RANKL and protects bone).
Cofactors Needed for Vitamin D to Build Bone
Nutrient | Role |
|---|---|
Magnesium | Required to convert vitamin D to its active form in liver and kidney; low magnesium increases RANKL and osteoclast activity. |
Vitamin K₂ (MK-7 / MK-4) | Activates osteocalcin and MGP so calcium is deposited into bone, not arteries; reduces osteoclast activity. |
Calcium + phosphate | Structural building blocks of bone mineral. |
Boron and potassium | Improve vitamin D signalling and reduce calcium loss. |
Individual Factors Matter — Bone Health Is Not One-Size-Fits-All
While vitamin D, magnesium, vitamin K and other nutrients play essential roles in bone building and bone remodelling, nutrient optimisation is only one part of the picture. Bone health is influenced by a wide range of individual factors, including:
Sex and life stage — bone density naturally declines with age, and women experience accelerated bone loss during perimenopause and menopause due to declining oestrogen (a hormone that protects bone).
Hormonal balance — low oestrogen, low testosterone, thyroid dysfunction, or high cortisol all affect bone turnover.
Activity level and mechanical loading — weight-bearing exercise stimulates osteoblasts (bone-forming cells).
Genetics and family history — influence vitamin D receptor (VDR) activity and fracture risk.
Lifestyle factors — stress, alcohol, smoking, medications (e.g., PPIs, corticosteroids) affect nutrient absorption and bone turnover.
If you would like to understand your personal nutrient status, hormone balance, vitamin D metabolism, book a consultation with me.
References:
Bikle, D.D. (2025) ‘Vitamin D: Production, Metabolism, and Mechanism of Action’, Available at: https://www.ncbi.nlm.nih.gov/sites/books/NBK278935/ (Accessed: 28 October 2025).
Bleizgys, A. (2024) ‘Zinc, Magnesium and Vitamin K Supplementation in Vitamin D Deficiency: Pathophysiological Background and Implications for Clinical Practice’, Nutrients, 16(6), p. 834. Available at: https://doi.org/10.3390/nu16060834.
Li, Y. et al. (2023) ‘Modulation of the vitamin D/vitamin D receptor system in osteoporosis pathogenesis: insights and therapeutic approaches’, Journal of Orthopaedic Surgery and Research, 18(1), p. 860. Available at: https://doi.org/10.1186/s13018-023-04320-4.
Liu, Y. et al. (2025) ‘Vitamin D and bone health: from physiological function to disease association’, Nutrition & Metabolism, 22, p. 113. Available at: https://doi.org/10.1186/s12986-025-01011-1.
Roseti, L. et al. (2024) ‘Nutraceuticals in osteoporosis prevention’, Frontiers in Nutrition, 11. Available at: https://doi.org/10.3389/fnut.2024.1445955.
Xu, D. et al. (2022) ‘Vitamin D inhibits bone loss in mice with thyrotoxicosis by activating the OPG/RANKL and Wnt/β-catenin signaling pathways’, Frontiers in Endocrinology, 13. Available at: https://doi.org/10.3389/fendo.2022.1066089.
Zhao, Y. et al. (2025) ‘Vitamins D and K jointly protect against osteoarthritis via regulating OSCAR during osteoclastogenesis’, Journal of Orthopaedic Translation, 52, pp. 387–403. Available at: https://doi.org/10.1016/j.jot.2025.03.018.
Zittermann, A. et al. (2025) ‘Association between magnesium and vitamin D status in adults with high prevalence of vitamin D deficiency and insufficiency’, European Journal of Nutrition, 64(1), p. 48. Available at: https://doi.org/10.1007/s00394-024-03559-9.
Blogs and Insights


